| Home Medical Index | First Posted: Apr 27, 2008 Jan 21, 2020 | |
Lyme Disease and Humans/More Comprehensive InformationSee also: Lyme Disease/Horses and Humans
Note: "Lyme Disease This is the most common tick-borne illness in the U.S. The CDC says there've been around 300,000 cases a year in recent years. The bacteria that causes it attacks your nervous system and possibly your heart, liver, eyes, and joints as well. Ticks that carry this disease live mostly in the Northeast and Upper Midwest. More than 95% of reported cases of Lyme disease were in those areas. (It gets its name from the town of Lyme, CT.) Lyme Disease Symptoms At first you may feel like you have the flu--fever, chills, a headache, and joint or muscle pain. You also may notice a skin rash that starts near the tick bite anywhere from 3 to 30 days later. As the rash gets bigger, the middle often clears and a red ring shows up around the outside, leaving a 'bull's-eye' look. About 60% of people who have it get this rash. Lyme Disease Treatment If you're in an area where the disease is common and find a tick on you, call a doctor right away, especially if the tick is fat. An antibiotic can keep you from getting Lyme disease if you take it within 72 hours of the bite. If you get the disease, your doctor will prescribe a longer antibiotics course. Most people fully recover, but symptoms can last more than 6 months. If it's not treated, you may get numbness in your arms or legs, or paralysis on one side of your face. There are many different types of ticks in the United States, and many of these ticks are capable of transmitting infections. Some infections are associated only with one type of tick's bite. The risk of developing these infections can depend upon the geographic location, season of the year, type of tick, and, most importantly, how long the tick was attached to the skin. While patients are often concerned about tick bites, the risk of acquiring a tick-borne infection is quite low, even if the tick has been attached, fed, and is actually carrying an infectious agent. Ticks transmit infection only after they have attached and then taken a blood meal from their new host. A tick that has not attached (and therefore has not yet become engorged from its blood meal) has not passed any infection. The risk of acquiring Lyme disease from an observed tick bite, for example, is only 1.2 to 1.4 percent, even in an area where the disease is common." The Guide to Tick-Born Diseases If a person has a tick bite, the clinician will likely advise one of two approaches:
Tick Identification and Lyme Disease Transmission
This link has an excellent visual example, with text explanations about the transmission of Lyme Disease. It provides a chart that shows the transmission time over a 3 day period, what the chances are of lyme disease transmission, and shows the changes in the size of the nymph from the beginning of its blood meal to its engorgement.
The Lyme disease bacterium, Borrelia burgdorferi, normally lives in mice, squirrels and other small animals. It is transmitted among these animals - and to humans - through the bites of certain species of ticks. In the northeastern and north-central United States, the black-legged tick (or deer tick, Ixodes scapularis) transmits Lyme disease. In the Pacific coastal United States, the disease is spread by the western black-legged tick (Ixodes pacificus). Other major tick species found in the United States have not been shown to transmit Borrelia burgdorferi. Black legged ticks transmit Lyme disease - Black legged (or deer) ticks (Ixodes scapularis and Ixodes pacificus) can transmit several tick-borne diseases including anaplasmosis, babesiosis and Lyme disease. An adult tick is pictured at left, though it is the smaller nymphal stage ticks which most commonly bite humans. 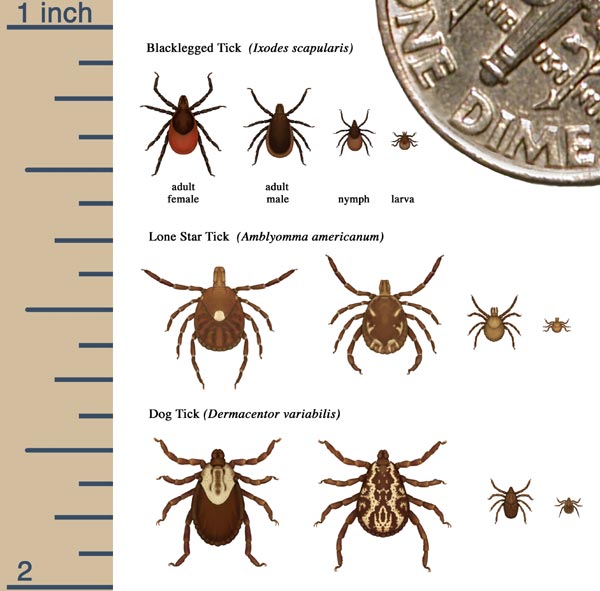  From right to left: An engorged adult deer tick, an adult before attaching to the skin, an engorged nymph (young tick), a nymph before it has attached. Both adults and nymphs can transmit Lyme disease.
Photograph Fred Dubbs
This image shows the stages and relative sizes of these tick species. Only the black legged ticks are known to transmit Lyme disease. Ticks not known to transmit Lyme disease - Lone star ticks (Amblyomma americanum) have been linked to transmission of ehrlichiosis, tularemia, and southern tick-associated rash illness (STARI). The saliva of these ticks is irritating, and can cause an allergic reaction at the site of the bite, American dog tick (Dermacentor variabilis) as well as the Rocky Mountain wood tick (Dermacentor andersoni) can transmit many diseases including Rocky Mountain spotted fever and tularemia. The history of the tick bite will largely determine which of these options is chosen. Before seeking medical attention, the affected person or household member should carefully remove the tick and make note of its appearance. I was at a seminar on Lyme Disease May 28, 2009, given by Sibley Hospital. It was excellent. In that seminar I learned that the most reliable lab to test for Lyme Disease is the Stonybrook Lab in New York I also learned that in the Washington, DC Metropolitan area there is a lab where you can send you tick to find out if it is carrying Lyme Disease. There is a charge, however, the name of the lab is Clongen Lab How To Remove A Tick
The proper way to remove a tick is using a set of fine tweezers and gripping the tick as close to the skin as is possible. The use of a smoldering match or cigarette, nail polish, Vaseline, or kerosene should be avoided, since they may irritate the tick and cause it to behave like a syringe, injecting organism-bearing bodily fluids into the wound. The proper technique for tick removal includes the following steps:
After the Tick Is Removed
Tick characteristics - It is helpful if the patient can provide information about the size of the tick, how difficult it was to remove, whether it was actually attached to the skin, if it was engorged (that is, full of blood), and how long it was attached. The size and color of the tick help to determine what kind of tick it was. The tick which transmits Borrelia burgdorferi (the bacterium that causes Lyme disease) and a number of other tick-borne infections in the northeast, midwest, and southeast United States is brown and approximately the size of a poppy seed or pencil point. Ticks that are black and about the size of a pencil eraser are more likely to be dog ticks. These ticks are not thought to carry Lyme disease, but can rarely carry Rocky Mountain spotted fever. A brown to black tick with a white splotch on its back is likely an Amblyomma americanum (Lone Star tick; named after the white splotch), which has been reported to spread a Lyme disease-like illness called STARI (southern tick-associated rash illness). A tick that was not attached, is still flat and tiny and is not full of blood, and was easy to remove or just walking on the skin, could not have transmitted Lyme disease or any other infection since it had not yet taken a blood meal. Only ticks that are attached and have finished feeding or are near the end of their meal can transmit the disease. After arriving on its host's skin, the tick that spreads Lyme disease usually takes 24 hours or more to attach to the skin. Even if a tick is attached, it must have taken a blood meal in order to transmit Lyme disease. At least 36 to 48 hours of feeding is required for a tick to have fed and then transmit the bacterium that causes Lyme disease. After this amount of time, the tick will be engorged (full of blood). An engorged tick has a globular shape and is larger than an unengorged one. The organism that causes Lyme disease, B. burgdorferi, lies dormant on the inner aspect of the tick's midgut. The organism becomes active only after exposure to the warm blood meal entering the tick's gut. Once active, the organism changes the proteins it produces and then enters the tick's salivary glands. As the tick feeds, it must get rid of excess water through the salivary glands. Thus, the tick will literally salivate organisms into the wound, thereby passing the infection to the host. Need for Treatment
The clinician will review the description of the tick along with any physical symptoms to decide upon a course of action. The Infectious Disease Society of America recommends preventive treatment with antibiotics only in patients who meet all of the following circumstances:
Monitoring for Lyme Disease
Many people have incorrect information about Lyme disease. For example, individuals may be concerned that Lyme disease is untreatable if antibiotics are not given early (this is untrue; even later features of Lyme disease can be effectively treated with appropriate antibiotics). Many local Lyme disease networks and national organizations disseminate unproven information and should not be the sole source of education about Lyme disease. Signs of Lyme Disease
Whether or not a clinician is consulted after a tick bite, the person who was bitten (or the parents if a child was bitten) should observe the area of the bite for expanding redness, which would suggest erythema migrans (EM), the characteristic rash of Lyme disease. The rash is usually a salmon color although, rarely, it can be an intense red, occasionally resembling cellulitis (infection of the skin). The color may be almost uniform. The lesion typically expands over a few days and is usually asymptomatic, although burning or itching has been reported. As the rash expands, it can clear in the center. The center of the rash can then appear a lighter color than its edges or the rash can develop into a series of concentric rings giving it a "bull's eye" appearance. In people with early localized Lyme disease, EM occurs within one month of the tick bite, typically within a week of the tick bite, although only one-third of people recall the tick bite that gave them Lyme disease. Components of tick saliva can cause a short-lived (24 to 48 hours) rash that should not be confused with EM. This reaction usually does not expand to a size larger than a dime. Up to 90 percent of patients with Lyme disease will develop EM; 10 percent of these may have multiple lesions. If EM or signs or symptoms suggestive of Lyme disease develop, the person should see a health care provider for proper diagnosis and treatment. Where to Get More Information
CDC Lyme Disease National Capital Lyme and Tick-Borne Disease Association This discussion will be updated as needed every four months on our web site Up to Date for Patients Your health care provider is the best source of information for questions and concerns related to your medical problem. Because no two patients are exactly alike and recommendations can vary from one person to another, it is important to seek guidance from a provider who is familiar with your individual situation. For Lyme Disease I would go to a doctor who specializes in infectious diseases. For More Information: Lyme Disease |