| Home Medical Index | First Posted May 14, 2010 Jan 21, 2020 | |
Nail in Horse Footby Debora JohnsonAs always, an enormous thank you to Kate. She gives the care and affection to our horses every day. When trauma or illness happen Kate is there administering all the care that the horses need. She always treats our horses as though they were her own. Bill and I trust her totally and want her to know that we are grateful to be able to have our horses at her place. I would like to add that Dr. Williamson has been there every step of the way. She, too, has been just wonderful. We are glad that she is available to us as a vet from Haymarket Equine Veterinary Practice.     The nail that I pulled out of A Patchy's frog. The coin is a penny for size comparison.
My husband, Bill and I were out at the Manassas Battlefield trail riding, enjoying each other, the beauty and history of the battlefield, and, of course, our horses when my horse, A Patchy, pulled up lame. He refused to take another step which is unlike him. He is usually forward moving and very much in tune with what I am asking him to do. In fact, I have trained him to five gaits by the use of verbal commands as well as by the placement of my body on his back. As Kate (A Patchy is boarded at Kate's) always says "A Patchy is NOT a rule breaker!" This behavior was totally out of character for him. I dismounted, my husband held the reins and I checked A Patchy's far, hind foot. What I found was nauseating! He had stepped on a nail that had penetrated the center of his frog. Horrible thoughts raced through my mind. I know that you are not suppose to take the nail out, however, we were in an area where no vet could access. We were also far away from the trailer and would have to somehow, walk out. The other risk was that trying to walk the horse out with the nail still in his foot might drive the nail even further into this dangerous sensitive area! I looked at the nail and where it had entered, made a mental note, placed my fingers underneath the square head of the rusty nail, held my breath, and gently applied backward pressure to dislodge the nail. It did not come out easily! I tried to make the area bleed, but it would not. Puncture wounds are not a good thing! And then, of course, there is the worry that the area will heal over on the outside leaving yuck on the inside to fester and infect. I asked A Patchy to walk forward as I led him with the reins. Once the nail was out he seemed to move soundly and willingly much to my surprise. We made it back to the trailer, loaded the two horses, and went immediately to the vet's office. We had tried to call but the number programmed into our phone did not seem to work. As luck would have it all of the vets were in the field. The staff at Haymarket Equine Veterinary Practice were wonderful. They immediately checked to see which vet was closest to our barn, apprised her of the situation and asked Dr. Williamsom to come ASAP to Kate's to help A Patchy. Bill and I took the horses back to the barn and readied them for the vet's arrival. I cleaned off A Patchy's foot and soaked it in warm water (We did not have any epson salts), then dried it off and put him in a well bedded stall. Dr. Williamson and the vet tech arrived within the hour. We advised her as to what had happened and showed her the nail. I determined that it did not go in more than 3/4 of an inch because taking into account the thickness of my fingers, the placement of my fingers under the nail head when extracting the nail, and the length of the nail that would seem about right. The nail penetrated the most troublesome part of the foot--the center of the frog where all of the major structure are located: coffin bone, navicular, bursa sack, ligaments, soft tissue, etc. The actual length of the nail measured 1 1/4" We think that the nail might date back to the Civil War and Kate is having a Civil War expert take a look at it. Note: "Puncture wounds from nails or other objects are in a whole different category and need to be treated much more aggressively. If possible the hoof is radiographed (X-rayed) with the nail or foreign object still embedded so that the direction and depth of the penetration can be determined. The object is removed and a contrast solution is injected into the penetration tract. This contrast solution appears as bright white on a radiograph. If the navicular bursa has been penetrated then the contrast solution easily drops into the bursa, and the entire bursa and penetration tract are bright white on the radiograph. If the bursa has been infected, then the horse is laid down under general anesthesia, and a section of the frog removed to expose the navicular bursa. At this time the bursa is flushed and treated at the site of infection. The area is kept open and flushed daily. The horse is put on strong antibiotics, and the hoof/open frog area is covered with a hospital plate (special shoe with a full metal plate covering the entire sole that can be removed and put back on). If all goes well, the bursa doesn't become infected, and the hoof fills in with scar and hoof material, which can take two to four months." Hoof Abscesses and Puncture Wounds 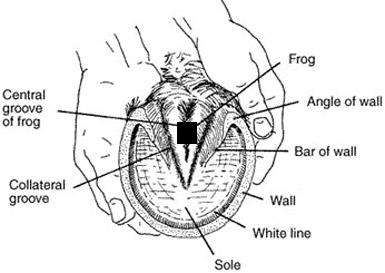 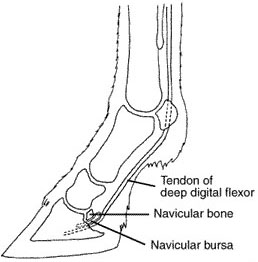  The first picture on your left shows the underside of the hoof. Both the first and second image come from the University of Missouri Extension and their permission to use notice allows me to have this on my site. Notice that I have made a black square to indicate where the nail went into A Patchy's foot. If you look to the picture on your right you will see how close all the internal structures are to that location. The centered picture below that is in color includes the coffin bone as well. The complexity of the horse's foot is sobering! Patient History (A Patchy Star)
May 7, 2010
Stepped on roofing nail while trail riding at Manassas Battlefield. Went into center of frog about 3/4 of an inch with over 1/2 length sticking out. Owner pulled since still well away from trailer and did not want to drive nail in deeper. Sound as soon as removed. Seen within 1-2 hours of stepping on nail. Walks sound, Dp wnl. No obvious trail but small brown slit in the plantar cleft of frog nearer the heel bulbs present but not able to probe tract. Cleaned area well, wrapped with sugardine. Discussed that since nail no longer in foot and no obvious tract that x-rays at this paint unlikely to determine extent of injury but if ANY lameness or fever we will need to take x-rays at this point. Discussed risks of deep abscess under frog and in digital cushion, as well as risk (though likely nail did not go deep enough to involve) of laceration of the deep digital flexor before insertion on the coffin bone as well as navicular bursa involvement. Gave 20 mfs Naxcel. Current on tetanus. Owner declines referral at this time.
The vet ran through the possible things we could do including taking A Patchy to Morven Park (Virginia Tech's Marion duPont Scott Equine Medical Center is a premier full-service equine hospital located in Leesburg, Virginia, that offers advanced specialty care, 24-hour emergency treatment and diagnostic services for all ages and breeds of horses. One of three campuses that comprise the Virginia-Maryland Regional College of Veterinary Medicine, the center and its team of equine specialists are committed to providing exceptional treatment for patients, superior service to clients and cutting-edge research to the equine industry.) or another Equine Hospital. I declined, and suggested that we do the most aggressive and proactive treatment that she (Dr. Williamson) felt would be in the best interest to A Patchy. The following is how we proceeded:  The vet tech, Sarah, making a wrap from duct tape.    &nb; &nb;  > >     May 10, 2010 Recheck
Walking sound 0.5/5 RH (right hind), mild increased pulse (Note: Normally, a resting horse has a pulse of 38 to 40 beats per minute. In resting horses, a heart rate over 80 can be a sign of a serious problem. If a calm horse has a pulse that is consistently over 60, it can also be a problem.) and mild heat in foot. Frog hard and not sensitive. No tract and no drainage. Bright. Per owner temp around 99 and has remained normal. No signs of lameness. Rewrapped magna paste. Already had Naxcel today. Temp was 100.5.
May 15, 2010 Recheck
Gaiting sound. DP (Digital Pulse) wnl (within normal limits), HT - Small amount of discharge from around frog in magna paste but wnl, no discharge from tract. Heel bulbs not sensitive. Mild bruising present on medial heel bulb. Temp 99.2. Since did had increased DP on last exam and very mild lameness want to continue antibiotics a little longer.
**About SMZ-TMP DS
"What is SMZ-TMP DS? SMZ-TMP (trimethoprim/sulfa) in double strength (DS) form is an antibiotic used to treat susceptible bacterial infections in multiple species. It can also be used to treat certain infections with protozoa. Who is it for? SMZ-TMP is for dogs and cats, plus other species as prescribed by a veterinarian. What are the benefits? * Broad-spectrum antibiotic treats a range of bacterial and protozoal infections, * Used for respiratory, urinary tract, skin or gastrointestinal infections and other conditions, * Trimethoprim works with sulfamethoxazole for better effectiveness SMZ-TMP is an antibiotic used to treat susceptible bacterial and protozoal infections. Trimethoprim makes sulfamethoxazole more effective. It is available in double strength tablets. How does SMZ-TMP work? This medication works by preventing the production of folic acid in bacteria. Without folic acid, bacteria cannot make essential proteins and will eventually die. Is there a generic equivalent available? SMZ-TMP DS is the generic equivalent of Bactrim and Septra. How is it given? SMZ-TMP is given orally, commonly with food. Encourage your horse to drink water when taking SMZ-TMP to prevent crystals from forming in the urine. Always follow the dosage instructions provided by your veterinarian. If you have difficulty giving the medication, contact your veterinarian. Use all of the medication prescribed, even if your pet appears well. If the entire course of treatment is not given, the infection may recur or worsen. What results can I expect? SMZ-TMP is absorbed well from the digestive system and is distributed to many body tissues, making it effective against infections in multiple organs. It is active against many different types of bacteria. It is usually given once or twice a day for a number of days. If doses are missed or the entire treatment regimen is not completed, the infection could recur or worsen. Consult your veterinarian if the animal's condition does not improve or worsens after beginning treatment with SMZ-TMP. What form(s) does it come in? This medication comes in tablet form..." SMZ A Patchy will be rechecked next Wednesday, May 19, 2010. I will update this article as soon as that visit has been completed and will give you the final disposition of A Patchy's progress the last week in May. May 19, 2010 Recheck
Today the vet and vet tech arrived at 10:00 am and did a recheck on A Patchy's foot and all over demeanor. They cut off the bandage wrap on his foot, checked the digital pulse in his foot (normal), looked for any oozing, swelling or heat in his foot or limbs (normal), took his temperature (normal), moved him in his gaits, on a lead rope, to see if there was any degree of lameness (normal), and did a basic wellness check on him. I was told to give him his last SMZs this PM. He is to be given probiotics for the next four days. For the next two days he may be turned out on the blue stones as long as the weather is dry and there is no mud. If those conditions are present he should remain in a clean stall. If there are no further symptoms, of any sort, including diarrhea, he may be turned out and resume his normal life! Of course, if any problems develop we are to call Dr. Williamson, immediately. I know that A Patchy, Kate, Bill and I will be very happy to see this day come! He has been an excellent patient and Kate, as always, has been the best. A big thank you to Haymarket Vet--everyone was so helpful. Dr. Williamson, a big thank you for being so professional and diligent in taking proactive and preventative measures in this matter. It seems to me that it is better to try to prevent any infection from occuring (a rusty nail penetrating the frog, etc. is NOT a good thing) rather than treat one after the fact. It has been difficult enough to "wait and see" under these carefully orchestrated, aggressive circumstances! Our human doctors should take notice and be as attentative! Hit it with a sledgehammer immediately and follow through. May 22, 2010- Bill and I are looking forward to getting back into the saddle, again. I know that Rusty and A Patchy are looking forward to getting back out on the trails. They love to go out--How do I know? They cannot wait to get on the trailer and go! They talk to us. May 25, 2010 - Bill and I trailered Rusty and A Patchy to the Manassas Battlefield and rode for two hours. The ground was soft, but not muddy. The footing was quite good. We took it easy and it appears that A Patchy has healed and is now out of the "danger zone." He has been off all antibiotics for one week now. He was given probiotics for 4 days after coming off the antibiotics. Don Roof, my farrier, is coming May 28th to take care of both horses's hooves. There is no sensitivity in the frog, bulbs, no heat in the hoof, digital pulse is within normal limits, there is no swelling, there is no lameness. A Patchy is happy to move along and was extatic to be out, once again. Everything appears to be back to normal. We are all so happy! July 30, 2010 - All is well! The heat wave broke today on this the hottest July on record in the Washington, DC area since records have been kept. Bill, his horse Rusty, A Patchy and I went riding today. It was heavenly--82 degrees and no bugs, footing was excellent. What a lovely day! Penetrating Injuries in Horse Hooves (AAEP 2010) "When it comes to penetrating hoof injuries, early, aggressive treatment is key to a favorable outcome, stressed Isabelle Kilcoyne, MVB, of the University of California, Davis, at the 2010 American Association of Equine Practitioners Convention, held Dec. 4-8 in Baltimore, Md. In a retrospective study she and colleagues examined complications, prognosis, and outcomes associated with penetrating foot injuries, particularly in the areas of the frog or the collateral sulci (clefts on either side of the frog). Penetrating foreign bodies confined to the frog or sulci can invade critical structures including the coffin bone, navicular bone, navicular bursa, deep digital flexor tendon sheath, and/or the coffin joint, noted Kilcoyne. All of the cases the team examined involved horses presenting with a nonweight-bearing lameness and diagnostic radiographs corroborating foot penetration. They graded each according to penetration depth:
|